Should I have the flu jab every year?
Over the winter months, many people catch flu. The NHS offers free vaccination to children, the over-65s and people at particular risk, like pregnant women and those with certain diseases. Yet less than two thirds of those eligible for the vaccination actually have it.

So why are people worried about the vaccine – and should you be?
A common reason for people declining the vaccine is that the previous year they had the jab and they actually believe it gave them flu.
This is not possible as there is no live virus in the vaccine. However, it takes about 7 – 14 days for your body to develop protection after the vaccine, so if you contract the flu during this time, or even in the week before, then you might not be fully protected.
Protection is important, because flu kills up to half a million people worldwide every year and during a pandemic, this can escalate to millions.
However, the flu virus presents huge challenges for health professionals tasked with selecting which vaccine to deploy in any given year, and for scientists developing new vaccines against it. This is because the virus is constantly changing, which makes it one of the most difficult diseases to predict and control.
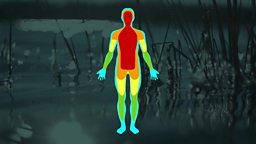
When we catch flu, what’s actually happening in our bodies is that the flu virus infects a cell, multiplies within the cell, then goes on to infect more cells. Over time our immune system learns to recognise the virus and starts to destroy it.
The flu vaccine offers protection by priming the immune system in advance. It does this by ‘training’ it to recognise particular protein molecules that exist on the outside of the virus (a bit like wrapping on a package), and destroy it.
However, the problem is that the proteins that make up this external ‘wrapper’ change frequently. When viruses multiply and copy their genetic material, sometimes tiny changes or errors occur, and this results in the virus mutating. The immune system may not recognise the altered proteins made by this mutated virus, and so it escapes detection and destruction.
So a new strain of the virus emerges, which can then infect cells and multiply, leading to more people catching it, and the cycle repeats.
To keep up with these mutations requires a huge ongoing research effort. Scientists have to constantly monitor the latest flu strains so they can update the vaccine.
This involves predicting which strains will be most common each winter, which is more successful some years than others. If the prediction is wrong, this can result in a less effective vaccine being deployed, leading to more cases of flu among the population.
However, it is always worth having the flu jab, though, because some protection is better than none at all.
Thanks to cutting edge research in virology, however, in future we may not need to be vaccinated every year. Researchers are working to create a new broad-spectrum or “Universal” flu vaccine, which will protect against more versions of the flu virus and last longer.
The principle behind the new vaccine is to target not the external ‘wrapper’ but instead specific protein molecules that lie deep inside the virus, which mutate much less frequently. If the immune system can learn to target proteins inside every strain, then it will be able to spot and destroy more types of flu. This could mean that even if a new strain comes along in the future, the vaccine should continue to work.
The researchers carrying out this work hope that people would need to be vaccinated less frequently than is currently the case, perhaps every 3 years and potentially up to every 5 years.
It is estimated that a Universal flu vaccine is still 5 - 10 years away. In the meantime, health professionals recommend that people should continue to use the currently available vaccine, especially for those at higher risk. (pregnant women, children, over-65 and those with certain medical conditions)
So if your GP recommends it, take the opportunity as it will help protect you, and those around you, and will not give you the flu.